Did you know that the structures inside your nose can permanently enlarge, blocking your airway even when you’re not sick? Turbinate reduction surgery addresses enlarged nasal structures that block airflow and cause chronic breathing difficulties. The inferior turbinates, finger-like projections inside your nose, normally warm and humidify incoming air. When these structures become permanently swollen, a condition called inferior turbinate hypertrophy ─ surgical intervention may restore normal breathing function.
The procedure reduces the size of enlarged turbinates through various surgical techniques, each targeting different tissue layers. Current turbinate reduction preserves the turbinate’s functions while creating more space for airflow. Surgery typically takes 30–60 minutes and can be performed alone or combined with septoplasty or sinus procedures.
Understanding Turbinate Anatomy and Function
The inferior turbinates sit along the outer walls of each nasal passage, extending from front to back. These structures contain bone covered by thick mucous membrane rich with blood vessels. The mucous membrane expands and contracts throughout the day, regulating airflow between nostrils in a process called the nasal cycle.
Turbinates filter particles from incoming air while adding moisture and warmth. The surface area created by these projections helps protect your lungs from dry, cold air and irritants. Blood vessels within the turbinate tissue can dilate or constrict based on environmental conditions, body position, and various triggers.
Inferior turbinate hypertrophy develops when the mucous membrane remains chronically swollen. The bone itself may also enlarge over time. This permanent enlargement differs from temporary swelling during colds or allergies, as the tissues lose their ability to return to normal size. The enlarged turbinates press against the nasal septum, blocking airflow even when inflammation subsides.
Surgical Techniques for Turbinate Reduction
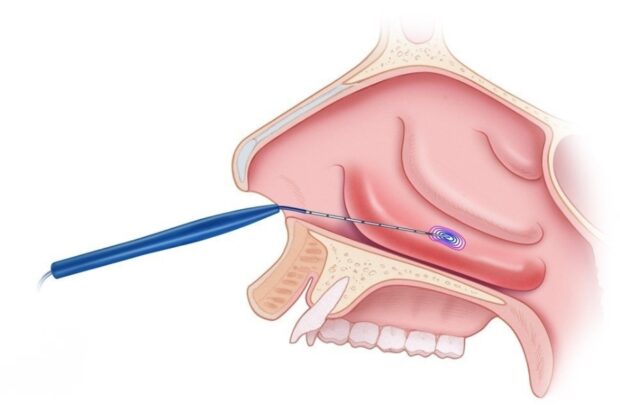
Radiofrequency Ablation
Radiofrequency ablation uses controlled heat energy to shrink turbinate tissue from within. The surgeon inserts a thin probe into multiple spots along the turbinate, delivering radiofrequency waves that create small areas of controlled damage. Over 6–8 weeks, the body reabsorbs this damaged tissue, reducing turbinate size while preserving the surface mucous membrane.
The procedure causes minimal bleeding since it doesn’t involve cutting the surface tissue. Patients experience gradual improvement as tissue shrinkage occurs over several weeks. Multiple treatment sessions may be needed to achieve results, particularly for severe hypertrophy.
Microdebrider-Assisted Turbinoplasty
This technique uses a specialized rotating instrument called a microdebrider to remove excess soft tissue while preserving underlying bone. The surgeon makes small incisions in the turbinate’s front portion, then carefully removes hypertrophied tissue layers. The microdebrider simultaneously cuts and suctions tissue, providing control over tissue removal.
The procedure maintains the turbinate’s natural contour while creating more nasal space. Recovery involves some crusting and congestion for 1–2 weeks as the surgical sites heal. The technique works well for soft tissue hypertrophy without significant bone enlargement.
Submucosal Resection

Submucosal resection removes bone and tissue from inside the turbinate while preserving the outer mucous membrane. The surgeon creates a small pocket within the turbinate, then removes portions of bone and erectile tissue. The preserved outer layer continues functioning normally while the reduced internal volume improves airflow.
This approach maintains the turbinate’s humidification and filtration capabilities. Healing occurs beneath the intact surface, reducing postoperative crusting. The technique addresses both bony and soft tissue components of hypertrophy.
Partial Turbinectomy
Partial turbinectomy removes a portion of the inferior turbinate, including the mucous membrane and underlying bone. The surgeon typically removes the lower or front portion, creating immediate airflow improvement. Current techniques preserve the upper portion to maintain some turbinate function.
This approach suits severe hypertrophy unresponsive to other methods. Careful technique prevents excessive removal, which could cause empty nose syndrome, a condition where patients feel unable to breathe despite open nasal passages.
The Surgical Process

Pre-operative assessment includes nasal endoscopy to evaluate turbinate size and identify concurrent issues like septal deviation or polyps. CT scans may reveal the extent of bony hypertrophy versus soft tissue enlargement. Allergy testing helps determine if allergic rhinitis contributes to turbinate swelling.
Surgery occurs under general anesthesia or local anesthesia with sedation, depending on the technique and whether additional procedures are planned. The surgeon accesses the turbinates through the nostrils, eliminating external incisions. Endoscopic visualization guides tissue removal or ablation.
Did You Know?
Turbinates can swell significantly during pregnancy due to hormonal changes affecting nasal blood vessels. This pregnancy rhinitis typically resolves after delivery without requiring surgical intervention.
Following tissue reduction, the surgeon may place dissolvable packing or splints to control bleeding and maintain turbinate position. Some techniques require no packing at all. The procedure concludes with careful inspection to ensure adequate airway opening without excessive tissue removal.
Post-operative care includes saline irrigation starting 24–48 hours after surgery. Patients use saline sprays or rinses 3–4 times daily to prevent crusting and promote healing. Pain medication manages mild discomfort, though many patients require only over-the-counter analgesics.
Recovery Timeline and Expectations

Initial recovery involves nasal congestion paradoxically worse than pre-operative symptoms. Swelling from surgical trauma temporarily blocks airflow more than the original hypertrophy. This congestion peaks around day 3–5, then gradually improves over 2–3 weeks.
Crusting develops as healing tissues form scabs inside the nose. Daily saline rinses help soften and remove crusts without disrupting healing. Your ENT specialist removes stubborn crusts during follow-up visits using instruments. Complete crust resolution typically occurs by week 4–6.
Important Note
Avoid blowing your nose forcefully for two weeks after surgery. Gentle sniffing and saline rinses safely clear nasal secretions without disrupting healing tissues.
Activity restrictions include avoiding strenuous exercise for two weeks to prevent bleeding. Light walking resumes immediately, with gradual return to normal activities. Patients typically return to work within 3–7 days, depending on their job requirements and comfort level.
Breathing improvement varies by surgical technique. Radiofrequency ablation shows gradual improvement over 6–8 weeks as tissue shrinks. Tissue removal techniques provide some immediate improvement once initial swelling subsides, with continued improvement over 3–6 months as healing completes.
Identifying Candidates for Surgery
Chronic nasal obstruction unresponsive to medical therapy represents the primary indication for turbinate reduction. Medical therapy includes:
- Intranasal corticosteroid sprays used consistently for at least 3 months
- Oral antihistamines for allergic components
- Environmental modifications to reduce allergen exposure
Physical examination findings supporting surgery include:
- Visible turbinate enlargement blocking more than half the nasal airway
- Turbinates that don’t shrink adequately with decongestant spray testing
- Contact between enlarged turbinates and the nasal septum
Endoscopic examination provides detailed visualization of posterior turbinate portions not visible through anterior rhinoscopy.
Associated symptoms strengthening the case for surgery include:
- Mouth breathing during sleep causing dry throat and dental problems
- Chronic sinusitis from impaired sinus drainage
- Recurrent nosebleeds from turbinate surface irritation
- Facial pressure or headaches from nasal obstruction
Sleep studies may document sleep disruption from nasal obstruction. Acoustic rhinometry or rhinomanometry objectively measures nasal airflow restriction, though clinical symptoms guide treatment decisions more than test numbers.
Risks and Potential Complications

Bleeding represents a common immediate complication, occurring in varying degrees. Minor bleeding stops with pressure and head elevation. Significant bleeding may require nasal packing or cauterization. Risk factors include blood-thinning medications, which should be discontinued before surgery according to your surgeon’s instructions.
Crusting persists longer in some patients, particularly smokers or those with dry environments. Prolonged crusting may indicate infection requiring antibiotic therapy. Regular saline irrigation and humidification minimize crust formation.
Empty nose syndrome, though rare with current techniques, occurs when excessive turbinate tissue removal eliminates normal nasal resistance. Patients paradoxically feel unable to breathe despite open nasal passages. Prevention involves conservative tissue removal preserving turbinate function.
Synechiae (adhesions) may form between the turbinate and septum during healing. These scar bands block airflow and require office-based division. Proper spacing during healing and regular follow-up visits prevent permanent adhesions.
Conclusion
Turbinate reduction offers effective treatment when medical therapy fails to address chronic nasal obstruction. Success depends on appropriate candidate selection, choosing the right surgical technique, and following proper post-operative care. Multiple surgical approaches exist to reduce turbinate size while preserving essential nasal functions.
If you are experiencing chronic nasal blockage, mouth breathing, or sleep disruption from enlarged turbinates, a MOH-accredited ENT specialist can evaluate your condition and discuss whether turbinate reduction surgery is appropriate for your specific case.